Real Stories, Real People, Real Strength
This space is for anyone living with, learning about, or supporting someone with an autoimmune disease. Here, we share real stories, honest emotions, and everyday wins — because healing feels lighter when we do it together. Whether you’re here to connect, listen, or lend your voice, you’re part of something bigger than a diagnosis.
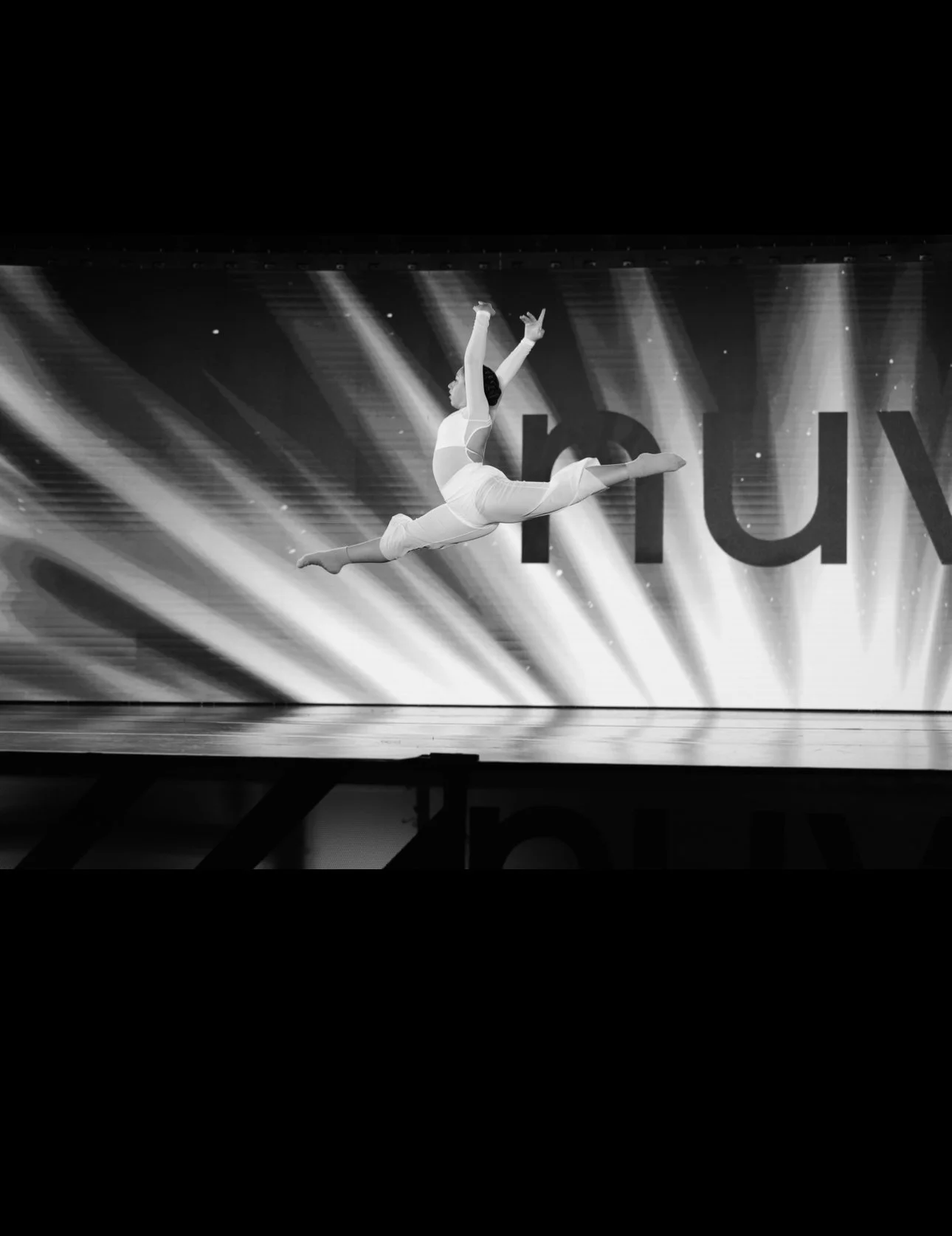
Gabby’s Story
UC, RA & POTS
I was 4 when I was diagnosed with Ulcerative Colitis. They had put me on many medication that did absolutely nothing for me until I was finally put on Remicade infusions and everything was smooth sailing from there or so I thought. At age 13 my doctor decided I was doing so well that I got go from every 4 weeks to every 6 week infusions. I thought that was amazing since I don’t have to go to the doctor as often until I was in so much pain. I do dance (mainly ballet) and it has always been my favorite thing to do since I started at age three but since the pain which was in my hip wouldn’t go away I had to stop. I went to many physical therapy places and had to take Tylenol constantly and it reached a point where I could barely walk. Later after an MRI scan it turned out I had Rheumatoid Arthritis in my hip joints. It felt reliving to hear since I had always known it was that even though people didn’t believe me. I had to stop dancing completely and I lost my sense of self. Dance was the only thing I was good at and loved to do. It had always been apart of my life that everyone knows me as “the dancer” and it was really heartbreaking to say goodbye to it. A year later I was feeling much better since I switched back to every 4 week infusions until I had started high school. My school is huge and all my classes are super far away from each other. I had developed some really abnormal symptoms like my heart racing for no reason, dizziness ,vertigo, nausea and all that fun stuff. I when to the doctor and was told that it was anemia and she gave me some iron pills and that was that. The doctor that I saw was not my normal doctor since she was on vacation but when my symptoms didn’t get better she told me it was POTS. It’s a daily struggle since I hide my pain so she’ll nobody understands when I can’t take it anymore and then I break down “you were fine a second ago” they would say. So many times I get so many stupid and unnecessary advice and comments about how I don’t need my accommodations like using the school elevator only used by teachers and staff. I know they have good intentions but nobody understands unless they have been through it too.
Skye’s Story
Kidney stones, Fibromyalgia, & Type II Diabetes
Hi! I’m Skye, no stranger to chronic illness, living with medullary sponge kidney with recurring kidney stones, fibromyalgia, and type II diabetes.
My story starts in 1st grade with chronic stomach issues that manifested itself into generalized anxiety disorder. My parents managed that as best they could through elementary school, and then came middle school. Sixth grade my anxiety was amplified due to being bullied which naturally caused my stomach issues to follow suit. I developed stomach ulcers, gastritis, and IBS-C. Forced by health to miss a lot of school, I was homeschooled my seventh grade year, but returned to school for eighth grade. What was supposed to be the most exciting time of entering high school, turned into my worst nightmare.
Struggling through the first semester of ninth grade with my stomach issues getting worse, I was still able to keep my gpa above 3.0. However, again, due to my continued missed days of school, I was forced to go online with my second semester of freshman year. In March, three months before the end of the school year and just two months after turning fifteen, I experienced the worst pain of my life, pain the doctors at the ER dismissed as constipation two days in a row. On the third day, they found a 4mm kidney stone.
My continued stomach issues required us to seek treatment at a larger hospital with more specialists at Helen DeVos is Grand Rapids. Throughout multiple visits over three years I went through a ton of different tests, submitted too many stool samples, survived several endoscopies, and many hated colonoscopies. I also qualified to participate in a brand new treatment for IBS that was only offered at a few hospitals called IB-stim. IB-stim is a treatment that uses electrical impulses to the cranial nerves through my ear. Unfortunately that treatment didn't work for me like my doctor had hoped. Before my last colonoscopy in Grand Rapids, my fecal calprotectant was extremely elevated, which means one of two things, Crohn's or Colitis. But once again, “everything came back looking good”.
As my sophomore year was approaching I still had high hopes of fulfilling my dreams of playing softball in college while becoming a physical therapist. But this life threw me into a medical field that I didn't ask for, learning what every lab means, understanding all the medical terms, researching all the medicine, knowing too much about my veins like how deep they are and which is best for poking, what buttons to push on all the machines, and becoming friends with nurses, doctors, cleaning personal, ultrasound techs, transporters, and cafe workers. Before long, I was trading dugouts for doctors’ offices, the crack of bats and the dust of softball diamonds gave way to the quiet hum of vital machines. My mitts and catchers gear were replaced by gowns, needle pricks, and the sterile glow of hospital corridors.
I was hospitalized several times over the next year with kidney stones. I went through my first lithotripsy and stent placement at 16. That stent placement sent me right back to the hospital as I couldn't pass any urine. That won me another stay in the hospital. Around the same time I started developing mouth ulcers, so painful I couldn't even brush my teeth, eat, or hardly drink.
Still not fully convinced I didn't have IBD, we opted for bigger and better, drove east about 4 hours to Cleveland Clinic. There I met with my gastroenterologist who ordered a capsule endoscopy to fully check for Crohn’s…..but, yep, you guessed it, “everything came back looking good”. I was then referred to Pediatric Rheumatology.
I was negative for Lupus and she wasn't sure it was Behcet’s, that is when I learned I was on the verge of an autoimmune disease and at this point they just started treating symptoms. I was put on Humaria for my mouth ulcers and that ultimately helped my gastro issue as well. I will sometimes still get a break through mouth ulcer but that's not been very often over the 2+ years I have been on this medicine.
However, I was still fighting kidney pain. In and out the ER, week after week, with them telling me my kidneys were full of stones but they weren’t blocking anything so they shouldn't be causing pain. Well, just because they shouldn’t, doesn't mean they don't. Again, not satisfied with the urologist and nephrologist’s conclusions, we headed back to Cleveland. I was put on two medicines to help stop the formation of kidney stones and diagnosed with medullary sponge kidney of both kidneys. Meaning, my kidney stones are not forming due to diet, drinking pop, and not enough water, like the local urologist tried to tell me, a 15 year old athlete. My kidneys will forever make stones because of their spongey nature. My urologist suggested doing a lithotripsy on both kidneys, separate times, to blast the stones in there that she can see. So, that is what I did.
February 21st my mom and I traveled to Cleveland Clinic to have this procedure done on the left kidney. What she found was a stone blocking one of the ducts of my kidney. She blasted it along with some other ones but needed to place a stent, unfortunately, that would be removed in a week. The pain afterward was unimaginable, which I remembered from the last one, and if anyone has ever had a ureter stent, we all say the same thing that it hurts worse than the kidney stone itself. But what I never expected to happen was being hospitalized locally, just five days later being the sickest I have ever been in my life, with sepsis. I was hospitalized for a week, with the stent still in, they were giving me heavy doses of Rocephin to kick the infection. I was able to go back to Cleveland on March 6th to have the stent removed. She explained that the stone itself carried the infection, and when she blasted it that's when the infection was released into my bloodstream. Which makes sense as to why I was so sick and in so much pain immediately following the procedure.
Scared out of my mind, I went back to Cleveland on April 11th to do the lithotripsy on the right kidney. This one worked out better than the last one, however I came home with a new diagnosis, Randall’s Plaque Syndrome. After getting my stent removed the pain was still just as excruciating. I was referred to switch from pediatric to adult rheumatology in Cleveland where I picked up another diagnosis of Fibromyalgia. But sadly my pain has never subsided, most days I feel like I am no longer living, I am just surviving.
Mara’s Story
Hypothyroidism, ulcerative colitis, rheumatoid arthritis and chronic migraines.
My health journey started at very young age. I got diagnosed with hypothyroidism when I was just a young child, i dont even remember life before I had it, I must have been 7 or 8 years old when I got the diagnosis.
As a child I thought it's so annoying that I need to take a pill every morning before breakfast, and every 12 months I needed to go see a doctor to make sure everything is still the same. I hated it. It made me gain weight and made it impossible to lose it, the headaches, fatigue, muscle cramps and other symptoms. But these were manageable with medication and overall life was fine.
But then my health decided that it wants to try something else now, as if life was too boring and easy how it was.
So, when I was 13 years old, turning 14, I got sick. I lost 20kg In 3 months, I couldn't eat anything, constant diarrhea, bloody stool, dizziness, fatigue, muscle weakness, headaches, my mother described my complexion as "wax doll".
One day I went to the doctor thinking it was just a weird stomach bug, and suddenly I was transferred to a bigger hospital, my hemoglobin was dangerously low, and infection markers high, I had been internally bleeding for months. I stayed at the hospital for the weekend to get blood transfusion and antibiotics to try to lower the infection markers.
Then came tests, like 20 vials of blood, colonoscopy, endoscopy, I swallowed a capsule camera to get imagining of my whole GI track. And I got diagnosed IBD, ulcerative colitis to be specific.
Then came medication trials, iron infusions, hospital stays. When my doctors realised that it's so bad that my body is unable to absorb oral medicine, they started biological medicine. I got it every two weeks intravenously, and the first kind was in use for 2 years.
During those two years I also got diagnosed with rheumatoid arthritis, which added medications, hospital stays for infections and cortisone shots to 16 joints at once, fortunately for me, I love needles.
Well, two years go by and no results, colonoscopy results and blood work results are just worse. So they suggested surgery, but I wasn't ready for that yet, my mental health was very bad, I was already suicidal so the thought of surgery was scary because I knew that I wasn't mentally ready for that, so they switched the medication and we tried for another 2 years.
Before my 18th birthday I had a colonoscopy, and it was so bad that my doctor thought she's looking at cancer, but fortunately biopsy came back negative.
After that colonoscopy, I requested to have the surgery, I was tired of going to the bathroom 20+ times a day, constantly in pain and tired.
So, 20/12/2022 I had my first surgery, just 18 days after I turned 18 years old. Laparoscopic colectomy was performed, they removed my entire colon, but left my rectum and anus. I got an illeastomy bag.
Recovery was interesting, not horrible but definitely not fun. I got used to the bag quickly.
The next two years was spent well, no pain, I gained weight back, I got used to taking care of my stoma and I felt like my life was back. During those years I also had time to choose if I wanted a permanent illeastomy bag or do I want to get a j-pouch surgery.
So when 2024 came around and I had to choose? I chose to keep my illeastomy bag, I had gotten attached to it and I felt comfortable with it, I didn't want to risk anything.
I had my second surgery 10/06/2024 and they removed my rectum and anus, no more bootyhole for me.
Recovery from that was worse than the first, mostly because I couldn't walk, sit or laugh without my butt hurting or stretching stitched. I also got nerve issues to my spine from the epidural that was used for pain management, it was placed wrong and caused damage.
The same year I got diagnosed with chronic migraines, after months and months of having almost daily migraines.
Now in 2025? Life is good. I can travel, date, work and study, exercise to some extent if my joint allow it, I still have some meds but it feels like nothing anymore.
I might have lost my teenage years to sickness, but now as a 21 year old, I am excited to spend my 20s as a capable young woman with manageable pain.
Nikita’s Story
Hashimotos
Growing I never felt like i truly got in with all the other kids. I was diagnosed with Hashimoto’s at 8 years old, and while other kids didn’t have many responsibilities, I had to make sure I took my medication every day, had to see multiple doctors multiple times a year, and had to get blood tests a lot. Being diagnosed at such a young age, I didn’t truly know why I had to do all this while the other kids didn’t. Growing up with this chronic illness wasn’t easy, I had to manage multiple symptoms, and everyday was a new challenge. This and multiple other reasons took a big toll on my mental health and I eventually got diagnosed with generalized anxiety disorder, clinical depression, and ADHD. I wasn’t able to talk to any of my friends or family about this because they wouldn’t understand how hard it was living with an autoimmune disease. There were some days where I didn’t want to wake up and wondered why my own body was fighting itself. Hashimoto’s is an autoimmune disease and a chronic illness that attacks the thyroid gland. While there is still no cure, the only thing we can do is manage the symptoms. It truly takes a big toll mentally and physically. But just know that while this journey can be challenging and daunting, you’re never truly alone.
Olivia’s Story
hEDs, dysautonomia, & mast cell activation syndrome
Hi! My name is Olivia, and this is my ongoing story of living with chronic illness.
Growing up, I was a dancer who loved to sing. As I got older, though, I began developing habits that eventually led to my diagnosis of anorexia in 2019. From that point on, life became a constant fight. Although my mental health journey is far from over, I’ve learned how to manage it and regain a sense of stability.
Around 2022, I started experiencing severe neck pain. At first, I dismissed it, assuming it came from years of playing volleyball, dance, and basketball in high school. But by 2023, the pain became unbearable. I found myself in the ER, unable to move my neck, with a pounding headache, yet I was sent home with only pain medication. This became a repeating cycle for the next three years and just got worse every time.
Fast forward to July 17th, 2025, everything changed. I went from boxing, lifting, and running miles a day to barely being able to stand. That night, I began shaking, sweating, and my jaw and neck locked up completely. At a new hospital, I finally received an MRI. The doctors noticed abnormalities but didn’t think they were immediately serious. They prescribed more medication, but it barely touched the pain.
Every day since has been a battle. I experience constant pain, limited movement in my neck, fainting spells, low blood sugar, nausea, vomiting, locked joints, and dislocations. After seeing a spine specialist, a physical therapist, and a specialist in the city, I was finally diagnosed with hypermobile Ehlers-Danlos Syndrome (hEDS), chronic pain, dysautonomia, and mast cell activation syndrome (MCAS). I remember crying when I got the diagnosis…someone finally believed me.
Because I was dismissed for so long, my neck tissue is now damaged and inflamed. The nerves from C1–C4 are being compressed, I have disc degeneration, and only about 10 degrees of neck movement. The vertigo is so severe that standing or walking for long periods is almost impossible. Somewhere along the way, I also developed hypoglycemia and now wear a continuous glucose monitor. We are still in the process of ruling out POTS and other potential complications.
There are days when I feel completely trapped in my own body, unable to move, speak, or even recognize myself. But I hold on to my goals. I’m a pre-med student, an intern, and I work hard every day to build the life I want. I’m surrounded by incredible friends and a family who have supported me through every step of this journey.
This is just a condensed version of my story…one filled with fear, uncertainty, grief, and resilience. I’ve learned that eating is a privilege, walking is a privilege, and living without pain is a privilege.
Be kind to yourself,to your body, to your mind, and to the life you have. You only get one (even if it’s a difficult one sometimes).
Kelseys Story
Rheumatiod Arthritis & Ankylosing Spondylitis
Hi! i’m kelsey. i’m a teenager living with chronic illness, and this is my story.
I live with Rheumatoid Arthritis and Ankylosing spondylitis. Here is what I would love to share. I’m no stranger to severe joint pain, chest pain, and stomach pain. The ER doctors and nurses have become very familiar with me. Diagnosed shortly after my sixteenth birthday with RA. A spell of passing out, with my limbs locking up lead to a hospitalization. Learning my immune system was attacking other parts of my body. This lead to a diagnosis of Ankylosing Spondylitis. I live with chronic pain, mostly affecting my hips and neck. Brain fog, weakness, fatigue. The list goes on. I’m sharing my story so others feel less alone, and awareness to illnesses affecting other, that often goes untreated. I take Methotrexate, essentially a chemo pill to slow down my progression. It takes its toll, but I am learning to live with this and enjoy my life through it all!
Liv’s Story
POTS
Growing up I was very athletic doing swimming & diving up into high school. in October of my junior year of high school (2021) l ended up in the mental hospital. After I left the hospital I started experiencing a high heart rate upon standing, lightheadedness, low blood pressure, extreme heat intolerance, exercise intolerance, pre syncope, fatigue, brain fog, and digestive issues. I was tired all the time. I slept 15 hours every night and took 3 hour naps during the day, still being extremely exhausted. In August of 2022, I ended up in the ER due to my symptoms for the first time. I was told i had “anxiety”. My symptoms were very manageable and stable for about a year. In the summer of 2023 I had a seizure and fainted for the first time. And after that I ended up back in the mental hospital. I was fainting nearly everyday. I was in chronic pain. I was tired. I was weak, most days not being able to dress myself. For another year, I made many hospital visits and left with no answers. I remember going on vacation with family in August of 2024 and had to stay in the hotel room bc I couldn't walk anymore. when I got back from tha vacation I found the neurologic wellness institute in Chicago where I went for 6 months. I did vestibular and neurological rehab. On the very first day, I was diagnosed with POTS. after I left I saw differences. I was less tired, had better balance, no more fainting, increase in time reaction, less dizziness; no more headaches, and i could even walk one mile without stopping. A year later I ended up on the mental hospital again. My health declined and I was in the ER for days a time and lost my full ability to walk leaving me using a walker, cane, and wheelchair. everyday my illness looks different. some days I can't go upstairs and some days I can walk one mile in 25 minutes. chronic illness does not discriminate, never take your health for granted. #curePOTS
Samantha’s Story
Psoriatic Arthritis
I am no stranger to a hospital, medications, or hospital routines in general. My 24-year-old son was born with chronic kidney disease and got a new kidney 8 years ago. So I was surprised when, almost 2 years ago, my body felt like it was not doing what I wanted anymore. I had surgery on both heels to remove bone spurs, and my feet never got better. I lost over 100 lbs, and still my joints felt the same. After seeing my first rheumatologist, they decided it was all in my head. My doc didn’t agree and sent me for a 2nd opinion, where I found out I indeed have psoriatic arthritis—started methotrexate shots every week and humriloz shots every other week. I would love to say that after 5 months, these shots are working, but that would be a lie. I have very high stress with my son’s health, my own health, and my 13-year-old daughter’s anxiety and struggles. Being a school bus driver does not help my stress level, but those little smiling faces keep me coming back for more! Most days I feel lost. I don’t know who I am anymore. Chronic pain and fatigue have consumed my life. The only thing I do anymore is work, come home, and go to bed. My husband of 27 years is losing his mind with me. My house is a complete wreck all the time. Most weekends, I am in bed recovering so I can start over on Mondays to do it all over again. I take naps almost daily. My medical bills are piling up, and to make matters worse, they are sure there may be another autoimmune condition, but they aren’t sure yet.
Possibly Crohn’s. Last thing I want or need. My 3 beautiful kids, Dakota, Hannah, and Laila, keep me trying whatever the doctors throw at me. Not to mention my love of being a school bus driver. The hardest part is the friendships I feel are lost and the disconnect with certain family members. Some make me feel like I’m not doing enough or that it’s really not that bad, she’s just over exaggerating. I would wish this on no one. I miss the me I used to be. I’m a caregiver by nature. I have always cared for my chronically ill son, and now, when I need care, it seems my son is the only one who gets it. I often think of finding Nemo when Dory says just keep swimming. That’s exactly what I’m doing! I am 49 years old and have lots of life left. I’m not done living. I just need to find what is gonna work and give me some of myself back. Thank you for listening. Stay strong, everyone!
Felicity’s Story
POTS & Orthostatic Hypotension
I’ve always been active. I grew up as a competitive swimmer with endless energy and a deep love for the water. But over time, I started noticing something wasn’t right. During races, I would suddenly feel dizzy and lightheaded, even though I was in great shape. At first, I brushed it off, thinking maybe I was overtraining or dehydrated, but the symptoms kept getting worse. After years of appointments, tests, and frustration, I was finally diagnosed with POTS (Postural Orthostatic Tachycardia Syndrome) and Orthostatic Hypotension (OH) about a year ago. Getting that diagnosis was both validating and overwhelming. It finally gave me answers, but it also meant facing a new reality that I couldn’t just push through anymore. Living with a chronic illness means even simple things can become challenges. Standing in line can make my heart race and my vision blur. Taking a shower can leave me completely drained. Some days I feel almost normal, and other days I have to cancel everything just to rest. Fatigue, dizziness, and brain fog are constant companions, and the emotional side can be just as hard, feeling misunderstood, learning to set boundaries, and adjusting to a slower pace when my mind still wants to move fast. Even though it’s difficult, I’m learning to accept rest, ask for help, and listen to my body. More than anything, I hope my story helps others feel seen and understood. Whether you’re still searching for answers or learning to live with a diagnosis, I want you to know your experience matters and that there is real strength in vulnerability.
Molly
Chronic recurring kidney stones, Urinary Retention, Pelvic Floor Dysfunction
I was sixteen when my life started revolving around hospitals instead of classrooms. What I thought was the worst pain of my life, turned into years of chronic kidney stones, urinary retention, cycles of catheters, pelvic floor dysfunction, daily antibiotics, and recovery. I learned medical terms most people never have to know, not because I wanted to, but because I had to. I thought the physical pain was the hardest hurdle, but losing grip of everything I once knew hurt worse. In fact, I wanted to be a nurse but the thought of dealing with medical tasks outside of my patient life felt daunting. I wanted to run from and escape it, not be more surrounded.
There were months when the emergency room felt more familiar than my own bed. The pain would come in waves so sharp it stole my breath, leaving me doubled over with nausea and exhaustion. Some days, I couldn’t sit through class without feeling the heavy ache in my back, where the school nurse and my guidance counselor became my lifelines. IV poles replaced backpacks, and my teammates moved on without me while I watched from hospital windows. I missed school dances, soccer games, and weekends with friends because my body had other plans. It’s hard to explain what it’s like when something as basic as using the bathroom becomes a daily challenge. When your body doesn’t cooperate, and every day feels like a test of patience and endurance. It may not even seem like a big deal to not be able to urinate normally, but it’s taken everything from me as I am unable to work and had to drop out of grad-school. I pass about 1-2 kidney stones a month, and have had multiple procedures and surgeries. It seems as though one problem leads to another. I also have IBS, possible Chrons and possible endometriosis (looking for a doctor that’ll listen and diagnose). As of late, I also have been getting a bunch of tests done for pancreatic cancer. Don’t have any results, but staying hopeful.
It’s hard to think about how long it’s been–6 years now! It makes me sad to think of how bad it’s gotten, but even in those moments, I found small victories. Getting through a day without pain meds. Laughing with a nurse who remembered my name. Passing a class I had to complete from a hospital bed. I learned to advocate for myself, to speak up when something felt wrong, to push for answers. Living with chronic illness has taken a lot from me, but it’s also given me perspective. I’ve learned that strength isn’t always loud; Sometimes it’s quiet, steady, and stubborn. It’s showing up to the next appointment, the next class, the next day, even when you were up all night feeling so sick and you’re tired of fighting. My journey hasn’t been easy, but it’s made me resilient in ways I never expected. I may carry this condition with me for the rest of my life, but I refuse to let it define who I am. Because even when my body feels fragile, my spirit isn’t, and that to me is its own kind of healing.
Tabby’s Story
Fibromyalgia
Fibromyalgia (Just the tip of the iceberg)
A word I had never even heard before suddenly became the label that defined me, or so I thought.
The day I was diagnosed, I thought it meant answers, maybe even hope. But instead, it marked the beginning of a battle I never asked for. A life where I woke up every morning in a body that felt eighty years old, trapped in pain that never took a break. My joints throbbed and burned as if they were filled with fire, my bones felt fragile and stiff, and even the smallest movements came at a cost.
Soon, I couldn’t go to school anymore. Online classes were my last grasp at normalcy, they started slipping through my fingers. My brain felt like it was underwater, words blurring and thoughts dissolving before I could catch them. The fatigue was bone-deep, the kind that no amount of sleep could touch.
I forgot what peace felt like.
What a day without pain felt like.
There were nights when the muscle spasms hit so violently that I screamed for someone, anyone, to help me but no one really could. Gabapentin. Muscle relaxers. Anti-inflammatories. Pills with promises that faded as fast as they came. Nothing dulled the pain for long.
Meanwhile, life moved on without me. My friends packed their bags for college, and started their adult lives while I stayed behind, in a room that felt smaller every day. The world I once belonged to now existed through screens and secondhand stories.
I spent a long time searching for reasons to keep going and some days, I still do. Chronic illness steals so much: your youth, your plans, your identity. It leaves you grieving the person you used to be while trying to make peace with the one you’ve become.
But here’s what I’ve learned, even when your world feels unbearably small, even when pain is all you’ve ever known, there is still strength in surviving. Every day I get through is one more day my illness doesn’t win. And though I may not remember what it’s like to live without pain, I’m learning what it means to live with it and that, somehow, is its own kind of victory.
Crystal’s Story
Hashimoto’s, Fibromyalgia, & Dysautonomia
You have Hashimoto’s, and it’s an incredibly difficult condition to treat,” my primary care doctor told me during a telemedicine appointment on my lunch break.
I had just taken a bite of my veggie sandwich in my freezing corporate office when she continued, “We have a long road ahead of us. Autoimmune diseases are tricky.”
Boy, was she right. And I wasn't prepared. Thyroid conditions run in my family, and I had been chasing a diagnosis for nearly a decade. Unfortunately, that wasn’t the end of the road. From there, I was referred to an endocrinologist, who then referred me to a rheumatologist, a neurologist, and even a cardiologist. This was all to rule out what might have developed from going so long without treatment.
Those appointments led to two more diagnoses: fibromyalgia and a form of dysautonomia. You see, these conditions often come in multiples — once you have one, others tend to follow. I don't just have one complex condition to manage; I have several. And as anyone with a chronic illness knows, the journey rarely ends there.
To top it all off, I lost my job. Between ER visits and missed workdays, I was let go from my corporate position. I remember thinking, Who would want to hire a chronically ill girl who keeps calling out?
But somewhere between the unknown and the exhaustion, a new thought began to form: If I can’t work for somebody else, why not work for myself?
I had been contemplating starting my own design business for a while — I didn’t think it would happen as soon as it did. I’m an architectural designer. The work is demanding and often stressful, but it’s also what I love. So I took the leap.
Now, in my first year as a business owner, I’ve worked on more projects than I ever did at any single company. I’m building my business between flare-ups. It’s not easy — but it’s worth it.
This story isn’t just about me, though. It’s about creating a space where people like me (people with chronic illnesses) can thrive. Through High Bar Designs, I’ve been able to hire others who also live with chronic conditions, including a drafting assistant and an administrative assistant who both understand what it means to work through flare-ups, fatigue, and unpredictability.
We are misunderstood... but certainly not unmotivated.
Together, we’ve built something that’s rooted in understanding, empathy, and excellence by giving each other grace, flexibility, and purpose.
At High Bar Designs, our motto is simple: If you take care of people, they’ll take care of you.
We’re setting the standard — and changing our little corner of the world, one project, one person, and one act of understanding at a time.
Olivia’s Story
Endometriosis & interstitial cystitis
If I had to describe living with chronic illness in one word, it would be exhausting. Not just physically, but mentally and emotionally too. For as long as I can remember, my body has always hurt in some way. As a kid, I thought that was normal, that everyone’s body ached, that fatigue was just part of growing up. Two years ago, I was finally diagnosed with fibromyalgia, and for a while, it felt like I finally had an answer. But it didn’t stop there. In December 2024, I started having constant pelvic pain that never went away. It got worse and worse until it became unbearable. After months of tests, appointments, and trying to convince doctors that something was seriously wrong, I was diagnosed in July 2025 with endometriosis and interstitial cystitis. Since then, every day has been a challenge. I’m still dealing with chronic pelvic pain every single day, and it’s exhausting in a way that’s hard to put into words. I’ve had so many labs, scans, and procedures that I’ve lost count. I recently had a colonoscopy that showed erosions in my small intestine, and I’m waiting to have an endoscopy to hopefully get more answers. On top of all that, I’m in college and working full-time, which is a lot to handle when your body is constantly fighting against you. Some days I can barely make it through a shift or finish schoolwork because the pain and fatigue are too much. Lately, I’ve even started considering applying for disability because working has become so hard for me. It’s something I never imagined I’d have to think about at my age, but chronic illness forces you to rethink what normal looks like. It feels like my life is a constant cycle of appointments, waiting rooms, and test results that never seem to end. There are days when I feel hopeful and strong, and days when I just feel completely drained. I’m learning how to live in the in-between, between pain and relief, between hope and disappointment, between wanting answers and being afraid of what they might be.
Kayla’s Story
MS
Honestly, I had no idea what an autoimmune disease even was until my own diagnosis and journey began. It started around June 2019, when I was 13 years old. My vision had become blurry, and my mom told me it was probably just from watching too much TV. One day, while we were on our way to the grocery store with the windows down, I remember feeling fine — until suddenly, everything went black for a split second. We thought I had just fainted from the heat and didn’t think much of it.
About a month later, as we were getting ready for bed, my mom noticed that my face looked lopsided. We went to the ER, and the doctors said it was Bell’s Palsy. I was prescribed medication and given an eye patch because I couldn’t close one eye. While the medication seemed to help at first, I started becoming very clumsy and losing my balance often.
We went back to the ER, where they told me it was vertigo and prescribed medication for that, but it didn’t help. Soon after, I had an appointment with my primary doctor because I kept falling. That morning, I lost some function in my legs and couldn’t get dressed by myself. My mom had to help me to the car, and by the time we arrived, I couldn’t even stand. I was sent to the Children’s Hospital of Augusta.
I don’t remember much after that until I was officially admitted. They ran neuro exams, CT scans, bloodwork, and MRIs. The scans showed lesions on my brain, so they did a spinal tap and diagnosed me with ADEM (Acute Disseminated Encephalomyelitis), another autoimmune disease. I was started on steroids and sent home with a taper. It worked for a little while—until it didn’t.
My symptoms came back, but worse. I was back in the hospital for two weeks, going through multiple tests, all negative except for what they already knew. They decided to do another spinal tap, which finally came back positive for MS. By then, I had missed most of 8th grade and was doing homebound schooling along with physical therapy three times a week. During that time, I had to relearn how to walk, talk, and even write again.
I was referred to a specialist and started taking Gilenya daily. It’s been almost six years since everything began, and thankfully, I’ve had minimal symptoms and flares. I’m forever grateful for that. My main symptoms now are fatigue, restless legs, soreness, and migraines.
I hope my story inspires others to share their own journeys and know that they are not alone in this battle.
Jules’s Story
Lupus
Almost 2 years ago, I was really sick, and the doctors kept telling me I just had a virus and it would go away on its own. i was told that for about 2 weeks. I got the COVID-19 vaccine a few weeks before this, so they assumed it was just a common reaction to a vaccine. Eventually things got so bad that my mom took me to the hospital where i got diagnosed with AKF( acute kidney failure). I was in the hospital for 2 months on treatment and different meds. I also was diagnosed with lupus. I still go to the hospital often for treatments, fluids, and tests. It’s hard, and I understand how u feel bc having a chronic illnem so sorry ’m so sorry u have to go through this too. ❤️
Molly’s Story
It all begins with an idea.
Anklyosing Spondylitis
For as long as I can remember, I thought exhaustion and pain were just things everyone dealt with. I was always active and motivated, the kind of person who powered through, until my body started sending me signals I couldn’t ignore. What began as stiffness in my back and random flare-ups of pain soon turned into days where even getting out of bed felt like a marathon.
Initially, I was told it was just stress, growing pains, or inflammation from overexertion. I bounced between doctors and specialists, explaining symptoms that didn’t seem to add up neatly on a chart. It was frustrating, not just the pain itself, but the feeling that I was constantly explaining myself and still being misunderstood.
After months (and countless appointments), I finally met a rheumatologist who listened — really listened. Blood tests, imaging, and a long conversation later, I got my diagnosis: ankylosing spondylitis, an autoimmune disease that causes inflammation in the spine and joints.
It was a strange mix of emotions, relief to finally have answers, but also fear of what that meant for my future. I remember sitting in my car afterward, letting the words sink in, realizing that my life would look different than I had planned — but that different didn’t have to mean less.
Since then, I’ve learned how to listen to my body, advocate for myself, and find community in others who understand the unspoken challenges of autoimmune life. My diagnosis isn’t my identity, it’s just part of my story. And that story has taught me strength, empathy, and the beauty of slowing down to care for yourself in ways you never thought you’d need to.
That’s why I started this space — to share real experiences, raise awareness, and remind others that even on hard days, we are never alone in this.